Major Depressive Disorder, a common mental health condition that has a profound impact on many people’s lives. Understanding the illness is an important first step toward recovery and a quality life.
What is Depression?
Depression is not just a temporary feeling of sadness or hopelessness, but a complex mental illness that affects your emotions, thoughts, behavior, and even physical function. People with depression experience feelings of sadness, hopelessness, or loss of interest in activities they used to enjoy for at least two weeks or longer. These symptoms are severe enough to interfere with daily life, work, school, and social interactions.
Depression can manifest in a variety of forms, from mild to severe. For example:
- Major Depressive Disorder (MDD): The most common form, with severe and persistent symptoms.
- Persistent Depressive Disorder (Dysthymia): A milder form of depression than MDD, but it can last for years.
- Postpartum Depression (PPD): This occurs in women after giving birth, who feel very sad, anxious, and hopeless.
- Seasonal Affective Disorder (SAD): Occurs during a specific season, such as winter, due to a lack of sunlight.
- Bipolar Disorder: A disorder characterized by extreme mood swings between mania and depression.
When does depression occur?
Depression can occur at any time, in people of all ages, races, social classes, and living situations. It can strike suddenly or develop gradually and without warning. Sometimes, it can be triggered by a traumatic life event, such as the loss of a loved one, job loss, financial problems, or chronic physical illness. Other times, it can occur for no apparent reason, leaving the sufferer and those around them confused.
What age group is most affected? Why?
In general, depression can occur at any age, but it is observed that adolescence and adulthood are the age groups most at risk of this disease.
Adolescence: This is a period when the brain is developing and there are strong hormonal changes. In addition, adolescents are faced with many pressures:
- Academic pressure: Exams, competition for high GPA
- Social pressure: Finding identity, recognition from friends, Bullying at school or on social media.
- Family problems: Parental divorce, family conflict, or excessive expectations from parents.
- Relationship problems: Breakups or strained relationships.
- Excessive use of technology and social media: Can lead to feelings of loneliness, comparing yourself to others, and decreased self-confidence.
Adulthood: This is a stage where individuals have to take on more responsibility in life. The main reasons that make this age vulnerable include:
- Work pressure: Too much work, strict bosses, competition, job loss or unsatisfactory work.
- Financial problems: Debt, daily expenses, lack of money.
- Relationship problems: Conflict with a partner, marital problems, divorce, loss of friends.
- Parenting: The pressure of being a parent.
- Chronic physical health problems: Diabetes, heart disease, cancer, or chronic pain.
- Traumatic life events: The loss of a loved one, loss of property, or other accidents.
- Lack of social support: Living alone, without a supportive family member, or having no close friends.
However, children and the elderly can also be at risk of depression. In children, it can present with symptoms that are different from those in adults, such as irritability, anger, not wanting to go to school, or frequent headaches or stomachaches for no apparent reason. In older people, it can often be hidden under other symptoms, such as forgetfulness, physical pain, or loss of appetite.
The reasons why adolescents and young adults are at higher risk are that they are going through many life changes, taking on more responsibility, and facing pressure from all sides. In addition, certain personality traits, such as overthinking, worrying excessively, or having high self-esteem, can also contribute to their vulnerability.
Symptoms of Depression
To be more specific, let’s look at the main symptoms of depression:
Psychological Symptoms:
- Feeling sad or irritable most of the time: No matter what happens, you still feel sad and unhappy. In children and adolescents, this may manifest as irritability or anger rather than sadness.
- Loss of interest or pleasure in activities you used to enjoy: Things that used to bring you joy become meaningless or boring.
- Feeling hopeless or worthless: Feeling useless or a burden to others.
- Feeling guilty or excessively blaming yourself: Blaming yourself for small things or events you didn’t cause.
- Difficulty concentrating, making decisions, or remembering: Decreased ability to think and concentrate.
- Thoughts of death or suicide: These are the most dangerous symptoms that require immediate attention.
- Excessive anxiety and fear: Unable to relax, constantly feeling uneasy.
Physical Symptoms:
- Sleep problems: Insomnia or hypersomnia.
- Appetite and weight changes: Rapid weight loss or gain for no apparent reason.
- Fatigue or loss of energy: Feeling tired most of the time, even after getting enough rest.
- Unexplained physical pain: Headaches, muscle aches, back pain, stomach pain that doesn’t respond to regular treatment.
- Slow or inactive body movements (psychomotor retardation): Slow speech, slow walking, slow task completion.
- Rapid or restless body movements (psychomotor agitation): Inability to sit still, shaky legs, shaky hands.
To diagnose depression, a specialist will assess the number of symptoms, the severity of the symptoms, and how long they have been present.
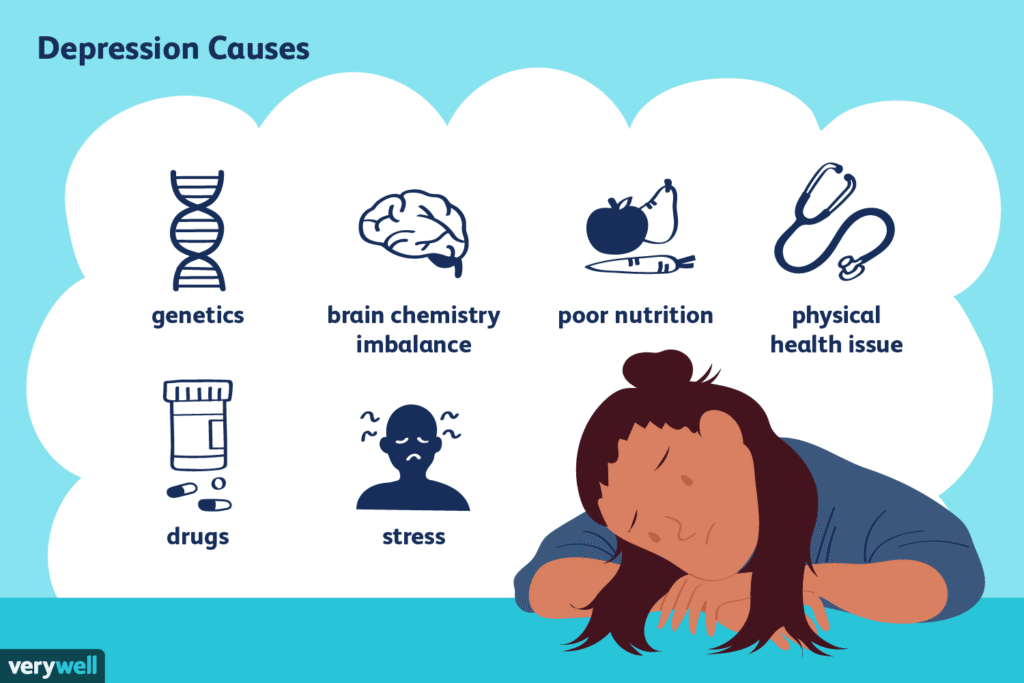
Causes of Depression
Depression is not caused by a single cause, but rather by a combination of factors:
Genetics: If a family member (such as a parent or sibling) has a history of depression, you are also at higher risk of developing the disease.
Biological Factors:
- Imbalance of chemicals in the brain (Neurotransmitters): Especially serotonin, norepinephrine, and dopamine, which play an important role in regulating mood, sleep, and appetite.
- Brain Structural Changes: Studies have shown that people with depression may have differences in the size or function of certain parts of the brain.
- Hormones: Hormonal changes, such as during pregnancy, postpartum, menopause, or thyroid disease, can also trigger depression.
Environmental and Life Events:
- Traumatic life events: Loss of a loved one, breakup, divorce, job loss, financial problems, abuse (physical, emotional, sexual).
- Chronic Stress: Work pressure, academic pressure, or ongoing family problems.
- Loneliness and lack of social support.
Psychological and Personality Factors:
- Negative thinking: Seeing everything in a negative way, overthinking, blaming yourself.
- Low Self-Esteem.
- Rigidity: Difficulty adapting to change.
- Childhood Trauma.
Medical Conditions: Some chronic illnesses, such as heart disease, cancer, diabetes, stroke, Parkinson’s disease, or HIV/AIDS, can also cause depression. Some medications can also have a depressant effect.
How to treat?
Treatment for depression must be comprehensive and tailored to each patient’s situation. There is no single treatment that is right for everyone. Common treatment methods include:
- Counseling/psychotherapy
Commonly known as “talking” therapy, which helps patients understand the thoughts, feelings, and behaviors that contribute to depression. Types of psychotherapy that are recommended include:
Cognitive Behavioral Therapy (CBT):
- Goal: Helps patients identify and change negative thoughts and behaviors. CBT teaches patients how to think positively and solve problems effectively.
- How to do it: Work with a therapist to identify negative thoughts (such as “I am worthless”) and replace them with positive thoughts (“I am capable”). It also helps patients set realistic goals and develop problem-solving skills.
Interpersonal Therapy (IPT):
- Goal: Focuses on solving problems in personal relationships and how those problems contribute to depression.
- How to do it: Helps patients improve communication skills, resolve conflicts, and build stronger relationships.
Problem-Solving Therapy:
- Purpose: Teaches the patient how to identify and solve real-life problems that cause stress.
- How to implement: Help the patient develop a step-by-step plan for solving the problem and implement it.
- Medication
Antidepressants can help correct chemical imbalances in the brain. The choice of medication depends on the patient’s symptoms, side effects, and response. Commonly used classes of medications include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Such as Fluoxetine (Prozac), Sertraline (Zoloft), Escitalopram (Lexapro). These are the first-line medications because they are highly effective and have few side effects. They work by increasing serotonin levels in the brain.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Such as Venlafaxine (Effexor) and Duloxetine (Cymbalta). They increase both serotonin and norepinephrine.
- Tricyclic Antidepressants (TCAs): Such as Amitriptyline and Imipramine. These medications are effective but have more side effects than SSRIs and SNRIs, so they are used less often today.
- Monoamine Oxidase Inhibitors (MAOIs): These are older medications that are highly effective but have dietary restrictions and many side effects, so they are used less often.
- Atypical Antidepressants: Other medications that are not SSRIs, SNRIs, TCAs, or MAOIs, such as Bupropion (Wellbutrin).
Important Note:
- Antidepressants are not drugs.
- They do not work immediately, and may take 2-4 weeks or longer to show full effect.
- Medications should be taken under the close supervision and guidance of a qualified medical professional.
- Do not stop taking your medication suddenly, even if you feel better, as this can lead to withdrawal symptoms and relapse.
- Complementary Therapies
In addition to the main treatments above, some complementary therapies may also help:
Lifestyle changes:
- Regular exercise: Helps increase endorphins, which are feel-good chemicals.
- Balanced diet: Eat foods that are good for the brain.
- Adequate sleep: Try to set a regular bedtime.
- Reduce alcohol and caffeine: These can make depression symptoms worse.
Quitting smoking.
- Practicing relaxation techniques: such as meditation, yoga, or deep breathing.
- Participating in social activities: Don’t isolate yourself, try to connect with friends or family.
- Setting small, realistic goals: To help boost your self-confidence.
- Getting enough sunlight: Especially for people with seasonal affective disorder (SAD).
- Maintaining physical health: Treating existing physical illnesses.
- Brain Stimulation Therapies
For severe cases or patients who don’t respond to medication or psychotherapy, doctors may consider brain stimulation therapies such as:
- Electroconvulsive Therapy (ECT): Uses a small electrical current to cause brief seizures, which can help correct brain chemicals. This method is very effective for severe cases, but requires careful monitoring.
- Transcranial Magnetic Stimulation (TMS): Uses a magnetic field to stimulate specific brain cells involved in emotions. This method is painless and does not require anesthesia.
- Vagus Nerve Stimulation (VNS): A small device that sends electrical impulses to the vagus nerve, which connects to the brain.
Who should you seek help from?
If you or someone you know is experiencing symptoms of depression, it is important to seek professional help.
- Psychiatrist: A medical professional who is qualified to diagnose, prescribe medication, and provide other treatments.
- Psychologist: A specialist who provides psychotherapy. They do not prescribe medication.
- Counselor/Therapist: Provides counseling and psychotherapy.
- General Practitioner: Can do an initial assessment and refer you to a specialist.
The Role of Family and Community
Support from family and friends is very important in recovering from depression.
- Listen carefully: Give them a chance to talk about their feelings without judgment.
- Encourage them to seek help: Help them schedule an appointment with a specialist and accompany them if possible.
- Help them follow their treatment plan: Encourage them to take their medication as prescribed and attend therapy sessions.
- Provide emotional support: Ensure they are not isolated.
- Don’t blame or criticize: Depression is not their fault.
Take care of yourself: Caring for someone with depression can be exhausting, so take care of yourself as well.


